Discuss Public Assistance Offered to Low Income Individuals and Families in Your Country
- Enquiry article
- Open Access
- Published:
The impact of social aid programs on population health: a systematic review of research in loftier-income countries
BMC Public Wellness book 19, Article number:2 (2019) Cite this commodity
Abstruse
Groundwork
Socioeconomic disadvantage is a cardinal cause of morbidity and mortality. One of the most important means that governments buffer the agin consequences of socioeconomic disadvantage is through the provision of social assistance. We conducted a systematic review of research examining the health impact of social assistance programs in loftier-income countries.
Methods
We systematically searched Embase, Medline, ProQuest, Scopus, and Web of Science from inception to Dec 2022 for peer-reviewed studies published in English-linguistic communication journals. We identified empirical patterns through a qualitative synthesis of the prove. We as well evaluated the empirical rigour of the selected literature.
Results
Seventeen studies met our inclusion criteria. Thirteen descriptive studies rated as weak (n = vii), moderate (north = four), and strong (n = two) found that social assistance is associated with agin health outcomes and that social assistance recipients exhibit worse health outcomes relative to non-recipients. Iv experimental and quasi-experimental studies, all rated as strong (n = 4), institute that efforts to limit the receipt of social assistance or reduce its generosity (likewise known equally welfare reform) were associated with agin health trends.
Conclusions
Evidence from the existing literature suggests that social help programs in high-income countries are failing to maintain the health of socioeconomically disadvantaged populations. These findings may in part reflect the influence of rest misreckoning due to unobserved characteristics that distinguish recipients from non-recipients. They may likewise point that the scope and generosity of existing programs are insufficient to offset the negative health consequences of astringent socioeconomic disadvantage.
Background
Decades of epidemiological research has demonstrated that socioeconomic resource such as wealth, income, and employment – oft referred to every bit the social determinants of wellness – are "primal causes" of health inequalities [1, 2]. They are fundamental in the sense that they influence the everyday atmospheric condition, experiences, and exposures that influence health status. Put simply, those with fewer socioeconomic resources get sicker and die sooner than those to a higher place in the socioeconomic hierarchy. These findings accept led to a broad consensus in the field of public wellness: social policies that shape the extent to which socioeconomic advantage and disadvantage occur in society offering the most constructive, if politically contentious, strategy for reducing health inequalities [three]. Indeed, the concluding report of the World Health Arrangement Commission on the Social Determinants of Health concluded that the emphasis in public health must shift from individual-level interventions that aim to modify people'due south behaviours to societal-level interventions that amend their everyday socioeconomic conditions [iv].
One of the most important means that societies intervene to buffer the agin consequences of socioeconomic disadvantage is through the provision of social assistance [v]. Social assistance refers to regime programs that provide a minimum level of income support to individuals and households living in poverty. These programs lend back up either in the class of straight greenbacks transfers or through a variety of in-kind benefits (e.g. food stamps and rent subsidies). Social assistance has been shown to strengthen the purchasing power of the poor and raise their textile standards of living [vi, 7]. From a public health bespeak of view, the supplemental provision of income can also enable people to avoid harmful exposures and adopt practices beneficial to their wellness [8]. Thus, theory predicts that social help programs offer an important means of protecting the health of socioeconomically disadvantaged groups and mitigating the extent of socioeconomic health inequalities [nine, 10].
While there is widespread theoretical support for the role of social assistance every bit a policy lever with which to meliorate population health and promote health disinterestedness, it is unclear what the extant prove demonstrates empirically. At the same time, there is growing concern that existing programs provide insufficient levels of protection and that such inadequacies in the social rubber net produce boggling costs, both human and economical [11,12,thirteen]. Such business has, in some cases, prompted calls for a major overhaul of traditional social assistance schemes. In Canada, Finland, and the netherlands, for example, governments accept conducted small-scale experiments to explore the potential benefits of culling systems of income provision, such as unconditional basic income [xiv]. At this critical juncture, there is a demand to have stock of the extent to which existing social assist programs are succeeding (or non) at promoting population wellness and health equity.
Given the clear implications of recent political developments for the health of socioeconomically vulnerable populations and the lack of clarity on the country of the extant show, our aim in this newspaper is to conduct a systematic review of peer-reviewed inquiry that has examined the health impact of social assist programs. We focus on programs that provide directly financial assistance rather than aid in the form of in-kind benefits. Previous reviews take evaluated the health impact of other sources of income maintenance, including food stamps [15], depression-income tax credits [16], minimum wage laws [17], and unemployment insurance systems [18]. Furthermore, to avoid overlap with similar reviews in low- and middle-income countries [nineteen], nosotros restrict our analysis to loftier-income countries with well-established welfare land systems (i.e. Commonwealth of australia, Austria, Kingdom of belgium, Canada, Kingdom of denmark, Republic of finland, French republic, Federal republic of germany, Hellenic republic, Republic of iceland, Ireland, Italy, Grand duchy of luxembourg, Netherlands, New Zealand, Kingdom of norway, Portugal, Spain, Sweden, Switzerland, United Kingdom, United States). To our knowledge, this is the showtime systematic review to evaluate the health touch on of social assistance transfers in high-income countries.
Methods
Search strategy
We conducted a systematic search of the literature in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The search protocol was registered with PROSPERO (CRD42016048078). The search terms are listed in Table 1. We searched the post-obit electronic databases from inception to December 31, 2017: Embase, Medline, ProQuest, Scopus, and Web of Science. We supplemented our electronic search by handsearching the reference lists of all included literature and related review manufactures. We restricted our search to English-linguistic communication publications in peer-reviewed scientific journals. Grey literature, working papers, and peer-reviewed commentaries defective direct empirical tests were excluded. Ii authors conducted split searches. Disagreements were resolved as a squad through discussion and consensus.
The initial search yielded 2058 unique articles. Abstracts were screened to make up one's mind their eligibility for full-text review. Eligibility was determined based on 4 inclusion criteria: (i) reference to a social aid programme; (ii) reference to a health outcome, major risk factor for disease (due east.thou. hypertension and obesity), or health behaviour (e.thou. smoking and nutrition); (iii) reference to an appropriate report population (i.e. working-age adults between 18 and 64 years of age); and (iv) reference to an empirical method of testing the wellness bear on of social assistance or social assistance reform. Nosotros excluded studies that examined health care outcomes (e.g. health insurance coverage and physician visits) which require a distinct theoretical orientation. Nosotros also excluded studies examining maternal and child health outcomes, equally these have been reviewed elsewhere [twenty]. Two authors marked each abstract as "Yes" if they satisfied all four inclusion criteria, "Maybe" if they satisfied two or three of the criteria; and "No" if they satisfied fewer than two of the criteria. Abstracts marked as "Aye" or with at least one "Maybe" were subject to full-text review.
Data extraction and analytic strategy
A standardized form was used to extract relevant data from the included studies. We extracted the following information from each study: championship, authors, yr of publication, country, data source, sample size, main research question, written report blueprint, health event, and main findings. Ii authors extracted the information independently. The results of the extraction were shared and discussed with the entire research team. Disagreements were resolved as a team through discussion and consensus. The extracted data was used to summarize the key features of the selected literature and synthesize the available bear witness across studies. The entire research team collaborated to identify empirical patterns based on this summary and synthesis.
Quality assessment
Nosotros assessed the quality of studies using a modified version of the Quality Assessment Tool for Quantitative Studies developed by the National Collaborating Centre for Methods and Tools. [21] Nosotros describe our method of assessment in greater detail in Additional file 1. We rated studies according to five criteria: (i) Did the study describe on a representative sample? (two) Did the written report describe the characteristics of the exposed and unexposed groups? (iii) Did the report adopt a descriptive cantankerous-sectional, descriptive longitudinal, quasi-experimental, or experimental study design? (4) Did the study control for important confounders such equally historic period, gender, marital status, and didactics? (v) Did the study certificate and account for attrition (only if longitudinal). On each criterion, studies were rated as either 'strong', 'moderate', or 'weak'. A global quality rating was derived based on whether studies had no weak ratings ('potent'), ane weak rating ('moderate'), or two or more weak ratings ('weak').
Results
Literature search
In Fig. 1, we summarize the results of our search strategy. Of the 2058 unique abstracts identified, eighty studies were selected for full-text review. Upon further examination, seventeen studies were constitute to encounter our inclusion criteria. Their primary characteristics are listed in Table 2 and described in further detail below.
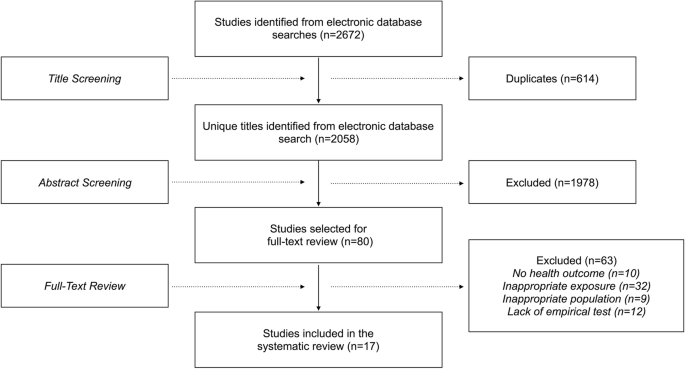
Summary of the search strategy and option procedure
Data sources and population characteristics
Most of the studies involved secondary analyses of nationally representative survey information [22,23,24,25,26,27,28,29,30,31,32,33,34,35]. Ii relied on population-based authoritative data [36, 37]. A final report drew from a smaller customs cohort report [38]. With respect to written report populations, ten of the studies looked at the general working-age population [22, 24, 25, 27, 29, 30, 32,33,34,35]. Another focused just on women [26]. Two restricted their analyses to socioeconomically disadvantaged individuals within the working-age population [36, 37]. The other four further restricted their analyses to socioeconomically disadvantaged women [23, 28, 31, 38]. The studies showed a high degree of geographic concentration. Ix of the seventeen studies were based in the United States [23, 26, 28, 31, 33, 34, 36,37,38]. Of the remaining eight studies, v were situated in other English-speaking liberal political economies characterized by weakly redistributive social policies, Commonwealth of australia, Canada, and the United Kingdom [24, 25, 27, 29, 35]. Two other single-land studies examined data from Norway and Sweden [22, 30]. Finally, 1 cross-national case study compared information from Germany, the United Kingdom, and the United States [32].
Policy exposures
Seven studies compared the health of social assistance recipients to that of their non-recipient counterparts in Canada, Norway, Sweden, and the United States [22, 24, 25, 28, 30, 35, 38]. Another ii examined the health bear upon of transitions in and out of social assistance recipiency [26, 29]. Four studies measured the health impact of modify in the coverage or generosity of social assistance programs in the United States, too known as welfare reform [23, 31, 36, 37]. Welfare reform ended guaranteed federal income support to poor families with children. They also imposed a lifetime limit on the receipt of public assistance and introduced new work-related eligibility requirements [39, 40]. Of the 4 studies examining the health bear on of welfare reform, 2 looked at the 1996 Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA) [23, 31], another looked at the 1994 Florida Family Transition Program (FFTP) [36], and the concluding looked at the 1996 Connecticut Jobs Starting time (CJF) initiative [37]. The final iv studies assessed whether social assist mitigates the adverse health consequences of unemployment past comparing jobless recipients and not-recipients [27, 32,33,34].
Study designs
Eight studies drew on a descriptive cross-sectional inquiry pattern [22, 24, 25, 27,28,29,thirty, 33, 35]. Another five studies employed a descriptive longitudinal inquiry pattern [26, 29, 32, 34, 38]. The final four studies exploited natural policy experiments to approximate the health impact of welfare reform. Two of these constructed quasi-experiments using departure-in-differences and synthetic control designs to compare alter in the health condition of policy-exposed and policy-unexposed groups before and after the implementation of PRWORA in the United States [23, 31]. Due to information limitations, neither of these quasi-experimental studies could place those who were directly affected by welfare reform. Rather, in both cases, the treatment group consisted of those the authors believed were near likely to have been afflicted; namely, socioeconomically disadvantaged unmarried mothers. The concluding two papers used policy experiments in Florida and Connecticut to examine the impact of welfare reform [36, 37]. Specifically, the authors compared mortality rates between a handling group that participated in the reformed social help plan and a control group that retained their traditional benefits.
Outcomes
Most of the seventeen studies investigated more than one relevant health result. More than half of the studies examined the impact of social assist on ane or more dimensions of mental health, including depression, common mental disorders, and adverse psychological symptoms [22, 24,25,26,27,28,29,30, 33,34,35, 38]. Five studies included self-rated health equally an upshot [31,32,33, 35, 38]. 3 explored health behaviours such as smoking, drinking, and nutrition [22, 23, 26]. Two studies focused on mortality [36, 37]. Another 2 looked at chronic atmospheric condition and major risk factors for disease such as hypertension and diabetes [35, 38].
Findings
All thirteen descriptive studies found that social assistance was associated with adverse health outcomes. Six cross-sectional studies (quality: weak) comparing the health of social assistance recipients to that of the general population found that recipients reported worse health outcomes than their non-recipient counterparts, fifty-fifty after adjusting for fundamental confounders [22, 24, 25, 28, xxx, 35]. In Australia, Canada, Sweden, Kingdom of norway, and the United States, social assist recipients reported higher levels of adverse psychological outcomes. The Canadian report also observed an association betwixt social assistance recipiency and higher rates of poor cocky-rated health (odds ratio (OR) 3.nine, 95% conviction interval (CI) 2.8–five.3). The Swedish and American studies found worse health behaviours among social help recipients, including higher rates of smoking, rampage drinking, and harmful dietary habits. In Sweden, for example, the odds of smoking were four.59 (95% CI iii.56–5.93) times higher among social assist recipients. Another four descriptive studies spanning iii countries (quality: weak or moderate) examined the role of social assist as a buffer against the agin health consequences of unemployment [27, 32,33,34]. All four studies failed to identify a protective effect. Rather, they plant that those who were unemployed and receiving social assistance reported worse self-rated health, a greater frequency of depressive symptoms, and a college charge per unit of psychological disorders. Of the remaining descriptive studies, 1 longitudinal analysis (quality: weak) of a small accomplice study in United States reported an association betwixt the receipt of social help during young or center adulthood and agin health outcomes 20 or thirty years later, including higher rates of poor self-rated wellness (OR 2.51, p < 0.05, no conviction intervals reported) [38]. The final two descriptive studies (quality: strong) investigated transitions in and out of social assistance in Australia and the U.s.a. and found that a motility into social assistance was associated with a higher frequency of depressive symptoms (β = 0.06, p < 0.05), worse mental health scores (β = − two.45, p < 0.001), and higher rates of binge drinking (OR two.06, p < 0.05, no confidence intervals reported) [26, 29].
All four experimental or quasi-experimental studies examining the health touch on of welfare reform in the United States found that such reforms were associated with adverse health trends. Ii studies examined the effects of PRWORA (quality: strong) and establish that welfare reform was associated with a 7% increase in the prevalence of poor self-rated wellness (95% CI i–12%), an 8.eight% increase in the prevalence of smoking (95% CI 6.8–10.8%), and an viii.3% increase in the prevalence of binge drinking (95% CI 14–nineteen%) amid the socioeconomically disadvantaged mothers most likely to have been directly affected [23, 31]. Another written report (quality: potent) constitute a 16% (95% CI 14–19%) college mortality rate among social help recipients who participated in the FFTP welfare reform experiment relative to a command grouping receiving the more traditional and generous prepare of benefits [36]. A like investigation of the CJF welfare reform experiment (quality: potent) found higher mortality rates among program participants, though, due in big office to small sample sizes, these estimates did non accomplish statistical significance [37].
Quality assessment
The results of the methodological quality assessment are presented in Table three. Seven studies were deemed to be low quality, 4 studies were moderate quality, and six studies were strong quality. The most common methodological consequence was the absence of an experimental or quasi-experimental study design that is capable, at to the lowest degree to some extent, of controlling for unobserved sources of confounding. But four of the studies were specifically designed to distinguish true policy effects from potential sources of selection bias that render a comparison of recipients and not-recipients problematic. Furthermore, though many of the studies controlled for the about common confounders (e.g. historic period, gender, marital status, household size, teaching), few explicitly accounted for the fact that a meaning majority of non-recipients are, past definition, ineligible for social assistance (e.g. due to incomes higher up means-test thresholds) and therefore serve as inappropriate controls.
Discussion
At that place are several important insights to be gained from our systematic review. Virtually notably, the results of our review suggest that social assist recipients tend to exhibit worse health outcomes relative to their non-recipient counterparts. This appears to be the case even after controlling for cardinal demographic and socioeconomic characteristics. This is somewhat puzzling, given that public health theory would predict that these programs are beneficial to health condition [1, 9]. The observation that those receiving benefits are faring worse than seemingly comparable non-recipients may reflect that there are, in fact, systematic differences between these populations that are not readily observable using the data upon which these studies rely. There are least 2 major sources of confounding that could be biasing the results of the reviewed studies. Firstly, individuals who endure from pre-existing health bug may exist selecting into social assist programs as a means of accessing coincident benefits that are otherwise out of accomplish (e.g. wellness insurance coverage). Secondly, pre-existing health problems may contribute to agin socioeconomic experiences such equally job loss which in turn predict social assistance status. Indeed, there is evidence suggesting that those who suffer from psychological problems have a greater likelihood of experiencing socioeconomic disadvantage and selecting into social help [41,42,43]. In a similar vein, findings from the extant literature indicate that problematic risk behaviours such as binge drinking may predict afterwards life socioeconomic hardship, thereby influencing social aid status [44, 45]. In addition, individuals with unreported textile resources such equally savings and family wealth may be opting out of, or be ineligible for, these benefits. In all three cases, these residue sources of confounding are likely to bias results towards a negative association betwixt income support and health status.
Alternatively, these findings may reflect the fact that social aid is increasingly conditional on a range of punitive, work-related obligations that compel entry into precarious employment weather condition [46,47,48]. While these measures have been shown to marginally amend employment outcomes amongst welfare recipients, the terms of their attachment to the labour market tend to be short-lived and produce their ain set of adverse socioeconomic consequences, including higher rates of in-work poverty [49]. In fact, recent evidence suggests that these precarious working conditions may pose an equal if not greater chance to health status than the experience of unemployment [50,51,52]. Based on these findings, we might expect social assistance programs that compel marginal labour market place zipper to produce negligible or fifty-fifty negative returns to health. Indeed, evidence from the broader literature demonstrates that culling income maintenance programs which place fewer behavioural requirements on recipients and provide more generous benefit levels than social assistance programs (e.g. unemployment benefits, earned income taxation credits, and unconditional cash transfers) have a positive outcome on individual health [53,54,55,56,57]. The finding here that social aid programs are non similarly associated with positive health outcomes may reflect that, unlike other forms of income maintenance, the scope and generosity of existing social assistance programs are insufficient to outset the negative health consequences of the astringent socioeconomic disadvantage that renders 1 eligible for such programs.
In contrast to the puzzling findings reported in descriptive studies, testify from experimental and quasi-experimental studies of welfare reform in the U.s.a. conform to our theoretical expectations. When benefits were reduced and work conditionalities were intensified, at that place were appreciable declines in the health condition of the socioeconomically disadvantaged groups who tend to be the principal recipients of welfare; namely, poor and low-educated single mothers. Welfare reform is frequently assumed to promote work and earnings by encouraging reattachment to the labour market. However, the results of existing evaluations advise that these returns are lukewarm at best [58, 59]. Furthermore, many households affected by welfare reform experienced heightened levels of material hardship [60]. Often, this was because women who were forced to go out welfare concluded upwards in low-paying, insecure jobs [61]. The results of our systematic review lend support to this view by demonstrating that these reforms accept had a negative bear on on health condition, an upshot that is sensitive to material conditions. Thus, while the main finding that social assistance programs do not appear to be succeeding at maintaining the health of the poor frustrates prevailing public health theory, our review provides some evidence suggesting that a reversal of these earlier welfare reforms and a resulting increment in the scope and generosity of social assistance benefits may have a positive effect on the health of socioeconomically disadvantaged populations.
At that place are several limitations to our assay. Commencement, we were not able to identify and include studies evaluating policy experiments involving the expansion of social assistance programs. Policy reforms in loftier-income countries take overwhelmingly involved the retrenchment of established levels of social protection [62,63,64]. Consequently, at that place are few examples of expansionary policymaking available for evaluation. 2nd, nosotros restricted our search to peer-reviewed journal manufactures. Evidence collected in books, reports, and working papers were excluded from the review. We also restricted our search to English-language publications. This may explain why most of the studies included in the review were from English-speaking countries characterized by relatively weak welfare state infrastructures, with a bulk being from the United States. Finally, due to heterogeneity across studies both in policy exposures and health outcomes, we were non able to conduct a meta-analysis of their results.
Conclusions
The overall results of our systematic review suggest that show on the health impacts of social help remains patchy. Rigorous evaluations of these programs are particularly defective. Few of the studies deemed for systematic differences between social assistance recipients and their non-recipient counterparts. Fewer still adopted the strongest available methods and study designs to evaluate the health effects of policies. We believe there are several principal reasons for the lack of available evidence on the question examined in this review. It may exist the instance that existing sources of data provide insufficient information for the conduct of rigorous policy evaluations. For example, population-based health surveys tend to provide little if any data on the benefit characteristics of respondents. In addition, while those working in the field of public health may be increasingly familiar with appropriate statistical techniques to evaluate societal-level policy interventions [65,66,67], social help programs may non be particularly amenable to the application of such methods. For case, many of the best available methods (east.g. regression discontinuity, divergence-in-differences, and interrupted time series designs) require researchers to identify moments of large-calibration policy alter. In contrast to other areas of public policymaking, such as tobacco or food labelling, social assistance programs are rarely affected past such sharp punctuations. A notable exception in this regard is welfare reform in the United States, for which there is show that we have reviewed here [23, 31, 36, 37]. Finally, institutional barriers associated with the deport of politically sensitive research may be standing in the style of the generation and dissemination of evidence on social assistance programs. Tackling the structural determinants of wellness requires large-scale government interventions (e.g. greater income redistribution and labour market regulation) [3]. Such efforts can attract opposition from political actors who oppose such a role for governments [68,69,lxx,71,72,73,74]. Many epidemiologists and other scientists contributing to the health inequalities literature may, in turn, feel that conducting and disseminating research of this nature is likewise political or, by virtue of the political opposition they believe information technology might face, likewise challenging to undertake [75, 76].
Withal these important challenges, there is a growing need for testify on the health furnishings of social assistance and similar social policies [77]. While governments frequently identify health equity as an important priority, their choice of interventions take largely relied on behavioural health promotion strategies that neglect to business relationship for the function of social policies as necessary levers to reduce health inequalities [78, 79]. Because efforts to eliminate or even reduce health inequalities are unlikely to be successful if they neglect to intervene upon their fundamental causes, it is imperative that public wellness researchers examine these policies and place the structural interventions that hold the greatest (and the to the lowest degree) hope for reducing health inequalities [80]. The paucity of such evidence is specially problematic in light of growing evidence that, despite more than a decade of efforts to promote wellness equity, inequalities in major indicators of population health appear to be widening [81, 82]. These troubling findings may reflect underlying changes in the social and economical architectures of high-income countries, such as the retrenchment of social protection policies – including social assistance programs [49, 62, 83] – and concomitant increases in agin socioeconomic experiences, such as poverty and unemployment [84, 85]. Taken together, these broader trends highlight a continuing need for solid evidence to align in support of interventions that target the key determinants of health.
Abbreviations
- CI:
-
Confidence interval
- CJF:
-
Connecticut Jobs First
- FFTP:
-
Florida Family Transition Plan
- OR:
-
Odds ratio
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PRWORA:
-
Personal Responsibleness and Work Opportunity Reconciliation Human activity
References
-
Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014;129:19–31.
-
Marmot One thousand, Friel South, Bell R, et al. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372:1661–9.
-
Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Geneva: World Health Arrangement; 2010.
-
Earth Health Organization. Endmost the gap in a generation: health disinterestedness through action on the social determinants of wellness: commission on social determinants of wellness final written report. Geneva: Earth Health System; 2008.
-
Bahle T, Pfeifer Chiliad, Wendt C. Social assist. In: Castles FG, Leibfried S, Lewis J, et al., editors. The Oxford handbook of the welfare country. Oxford: Oxford University Press; 2010.
-
Nelson K. Mechanisms of poverty alleviation: anti-poverty effects of non-ways-tested and means-tested benefits in 5 welfare states. J Eur Soc Policy. 2004;fourteen:371–90.
-
Kenworthy Fifty. Do social-welfare policies reduce poverty? A cross-national cess. Soc Forces. 1999;77:1119–39.
-
Phelan JC, Link BG, Tehranifar P. Social conditions equally fundamental causes of wellness inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51:S28–xl.
-
Nelson Thousand, Fritzell J. Welfare states and population health: the function of minimum income benefits for mortality. Soc Sci Med. 2014;112:63–71.
-
Lundberg O, Yngwe MÅ, Stjärne MK, et al. The role of welfare state principles and generosity in social policy programmes for public health: an international comparative study. Lancet. 2008;372:1633–40.
-
Ruckert A, Labonté R. Health inequities in the age of austerity: the need for social protection policies. Soc Sci Med. 2017;187:306–eleven.
-
Morgen S, Acker J, Weigt J. Stretched thin: poor families, welfare piece of work, and welfare reform. Ithaca: Cornell University Printing; 2013.
-
Nelson K. Social assistance and and Eu poverty thresholds 1990-2008. Are European welfare systems providing just and fair protection against low income? Eur Sociol Rev. 2013;29:386–401.
-
Segal H. Finding a better way: a basic income pilot project for Ontario. Toronto: Government of Ontario; 2016.
-
Black AP, Brimblecombe J, Eyles H, et al. Nutrient subsidy programs and the health and nutritional status of disadvantaged families in loftier income countries: a systematic review. BMC Public Health. 2012;12:1099.
-
Pega F, Carter K, Blakely T, et al. In-piece of work tax credits for families and their impact on wellness status in adults. Cochrane Database Syst Rev. 2013;half-dozen:CD009963.
-
Osypuk TL, Joshi P, Geronimo K, et al. Practise social and economic policies influence health? A review. Curr Epidemiol Rep. 2014;1:149–64.
-
Renahy E, Mitchell C, Molnar A, et al. Connections between unemployment insurance, poverty and wellness: a systematic review. Eur J Pub Health. 2018;28:269–75.
-
Lagarde M, Haines A, Palmer N. The bear on of provisional cash transfers on health outcomes and utilize of wellness services in low and heart income countries. Cochrane Database Syst Rev. 2009;7:CD008137.
-
Glassman A, Duran D, Fleisher Fifty, et al. Impact of conditional cash transfers on maternal and newborn health. J Wellness Popul Nutr. 2013;31:S48–66.
-
National Collaborating Eye for Methods and Tools. Quality cess tool for quantitative studies. Hamilton, ON: McMaster University; 2017.
-
Baigi A, Lindgren E-C, Starrin B, et al. In the shadow of the welfare society ill-health and symptoms, psychological exposure and lifestyle habits amid social security recipients: a national survey study. Biopsychosoc Med. 2008;2:15.
-
Basu Southward, Rehkopf DH, Siddiqi A, et al. Health behaviors, mental wellness, and health intendance utilization amid unmarried mothers after welfare reforms in the 1990s. Am J Epidemiol. 2016;183:531–8.
-
Butterworth P. The prevalence of mental disorders amid income support recipients: an of import consequence for welfare reform. Aust NZ J Pub Health. 2003;27:441–8.
-
Butterworth P, Burgess PM, Whiteford H. Examining welfare receipt and mental disorders after a decade of reform and prosperity: analysis of the 2007 National Survey of mental health and wellbeing. Aust NZ J Psychiat. 2011;45:54–62.
-
Dooley D, Prause J. Mental health and welfare transitions: depression and alcohol abuse in AFDC women. Am J Community Psychol. 2002;thirty:787–813.
-
Ford E, Clark C, McManus S, et al. Common mental disorders, unemployment and welfare benefits in England. Public Health. 2010;124:675–81.
-
Jayakody R, Danziger S, Pollack H. Welfare reform, substance use, and mental health. J Wellness Polit Policy Police force. 2000;25:623–52.
-
Kiely KM, Butterworth P. Social disadvantage and private vulnerability: a longitudinal investigation of welfare receipt and mental health in Australia. Aust NZ J Psychiat. 2013;47:654–66.
-
Løyland B, Miaskowski C, Dahl E, et al. Psychological distress and quality of life in long-term social help recipients compared to the Norwegian population. Scand J Soc Med. 2011;39:303–11.
-
Narain Chiliad, Bitler M, Ponce N, et al. The touch on of welfare reform on the wellness insurance coverage, utilization and wellness of depression pedagogy single mothers. Soc Sci Med. 2017;180:28–35.
-
Rodriguez E. Keeping the unemployed salubrious: the consequence of ways-tested and entitlement benefits in Britain, Federal republic of germany, and the United States. Am J Public Wellness. 2001;91:1403–11.
-
Rodriguez Eastward, Lasch K, Mead JP. The potential role of unemployment benefits in shaping the mental health impact of unemployment. Int J Wellness Serv. 1997;27:601–23.
-
Rodriguez Due east, Frongillo EA, Chandra P. Exercise social programmes contribute to mental well-being? The long-term impact of unemployment on low in the United States. Int J Epidemiol. 2001;xxx:163–70.
-
Vozoris NT, Tarasuk VS. The wellness of Canadians on welfare. Tin can J Public Wellness Rev Can Santee Publique. 2004;95:115–20.
-
Muennig P, Rosen Z, Wilde ET. Welfare programs that target workforce participation may negatively bear upon mortality. Health Aff. 2013;32:1072–7.
-
Wilde ET, Rosen Z, Couch K, et al. Affect of welfare reform on bloodshed: an evaluation of the Connecticut jobs outset program, a randomized controlled trial. Am J Public Wellness. 2014;104:534–8.
-
Ensminger ME, Juon H-S. The influence of patterns of welfare receipt during the kid-rearing years on later physical and psychological health. Women Health. 2001;32:25–46.
-
Bare RM. Evaluating welfare reform in the United states of america. J Econ Lit. 2002;twoscore:1105–66.
-
Gilbert N. Transformation of the welfare state: the silent surrender of public responsibility. Oxford: Oxford University Press; 2002.
-
Andreeva Eastward, Hanson L, Westerlund H, Theorell T, Brenner MH. Depressive symptoms equally a cause and effect of task loss in men and women: evidence in the context of organisational downsizing from the Swedish longitudinal occupational survey of wellness. BMC Public Wellness. 2015;fifteen:1045.
-
Callander EJ, Schofield DJ. Psychological distress and the increased risk of falling into poverty: a longitudinal study of Australian adults. Soc Psychiatry Psychiatr Epidemiol. 2015;50(10):1547–56.
-
Kiely KM, Butterworth P. Mental health selection and income back up dynamics: multiple spell discrete-time survival analyses of welfare receipt. J Epidemiol Community Health. 2014;68:349–55.
-
Tucker JS, Orlando M, Ellickson PL. Patterns and correlates of rampage drinking trajectories from early boyhood to young adulthood. Health Psychol. 2003;22:79–87.
-
Viner RM, Taylor B. Adult outcomes of binge drinking in adolescence: findings from a UK national birth cohort. J Epidemiol Community Health. 2007;61:902–7.
-
Peck J. Workfare states. New York: Guilford Press; 2001.
-
Deeming C. Rethinking social policy and guild. Soc Policy Soc. 2016;15:159–75.
-
Benach J, Vives A, Amable K, et al. Precarious employment: agreement an emerging social determinant of health. Annu Rev Public Health. 2014;35:229–53.
-
Segal E. The promise of welfare reform: political rhetoric and the reality of poverty in the twenty-starting time century. New York: Routledge; 2012.
-
Butterworth P, Leach LS, McManus Southward, et al. Common mental disorders, unemployment and psychosocial chore quality: is a poor task amend than no chore at all? Psychol Med. 2013;43:1763–72.
-
Chandola T, Zhang N. Re-employment, job quality, wellness and allostatic load biomarkers: prospective show from the UK household longitudinal study. Int J Epidemiol. 2018;47:47–57.
-
Kim TJ, von dem Knesebeck O. Is an insecure task better for health than having no job at all? A systematic review of studies investigating the health-related risks of both job insecurity and unemployment. BMC Public Wellness. 2015;15:985.
-
Evans WN, Garthwaite CL. Giving mom a break: the impact of higher EITC payments on maternal wellness. Am Econ J. 2014;6(ii):258–90.
-
Pega F, Walter S, Liu SY, et al. Unconditional cash transfers for reducing poverty and vulnerabilities: effect on employ of wellness services and wellness outcomes in low and middle-income countries. Cochrane Database Syst Rev. 2014;8:CD011247.
-
Rehkopf DH, Strully KW, Dow WH. The short-term impacts of earned income tax credit disbursement on wellness. Int J Epidemiol. 2014;43(vi):1884–94.
-
O'Campo P, Molnar A, Ng East, et al. Social welfare matters: a realist review of when, how, and why unemployment insurance impacts poverty and health. Soc Sci Med. 2015;132:88–94.
-
Thornton RL, Glover CM, Cené CW, et al. Evaluating strategies for reducing health disparities by addressing the social determinants of health. Wellness Aff. 2016;35(viii):1416–23.
-
Eichhorst W, Kaufmann O, Konle-Seidl R. Bringing the jobless into work?: experiences with activation schemes in Europe and the US. New York: Springer; 2008.
-
Danielson C, Klerman JA. Did welfare reform crusade the caseload reject? Soc Serv Rev. 2008;82:703–xxx.
-
Danziger S, Heflin CM, Corcoran ME, et al. Does it pay to move from welfare to work? J Policy Anal Manage. 2002;21:671–92.
-
Corcoran M, Danziger SK, Kalil A, et al. How welfare reform is affecting Women's work. Annu Rev Sociol. 2000;26:241–69.
-
Béland D, Daigneault P-M. Welfare reform in Canada: provincial social assistance in comparative perspective. Toronto: University of Toronto Press; 2015.
-
Hacker JS. The keen risk shift: the new economic insecurity and the reject of the American dream. Oxford: Oxford University Printing; 2008.
-
Betzelt Southward, Bothfeld Southward. Activation and labour market place reforms in Europe: challenges to social citizenship. New York: Springer; 2011.
-
Basu Southward, Meghani A, Siddiqi A. Evaluating the health impact of large-scale public policy changes: classical and novel approaches. Annu Rev Public Wellness. 2017;38:351–70.
-
Craig P, Katikireddi SV, Leyland A, Popham F. Natural experiments: an overview of methods, approaches, and contributions to public health interventions. Annu Rev Public Health. 2018;39:39–56.
-
Handley MA, Lyles CR, McCullough C, Cattamanchi A. Selecting and improving quasi-experimental designs in effectiveness and implementation inquiry. Annu Rev Public Health. 2018;39:5–25.
-
Baum Atomic number 26, Laris P, Fisher G, et al. "Never mind the logic, give me the numbers": former Australian health ministers' perspectives on the social determinants of health. Soc Sci Med. 2013;87:138–46.
-
Braveman P, Egerter Due south, Williams DR. The social determinants of wellness: coming of age. Annu Rev Public Health. 2011;32:381–98.
-
Embrett MG, Randall GE. Social determinants of health and health disinterestedness policy research: exploring the use, misuse, and nonuse of policy analysis theory. Soc Sci Med. 2014;108:147–55.
-
Frieden TR. A framework for public health action: the wellness impact pyramid. Am J Public Wellness. 2010;100(four):590–5.
-
Goldberg D. In support of a broad model of public wellness: disparities, social epidemiology, and public health causation. Public Wellness Ethics. 2009;2(1):70–83.
-
Pickett Yard, Wilkinson R. The Spirit level: a example written report of the public dissemination of health inequalities research. In: Smith KE, Bambra C, Hill SE, editors. Wellness inequalities: critical perspectives. Oxford: Oxford University Press; 2015.
-
Raphael D, Curry-Stevens A, Bryant T. Barriers to addressing the social determinants of health: insights from the Canadian experience. Health Policy. 2008;88(2–3):222–35.
-
Douglas M. Beyond 'health': why don't we tackle the cause of wellness inequalities? In: Smith KE, Bambra C, Hill SE, editors. Wellness inequalities: critical perspectives. Oxford: Oxford University Printing; 2015.
-
Muntaner C, Chung H, Tater Grand, et al. Barriers to cognition production, cognition translation, and urban health policy change: ideological, economical, and political considerations. J Urban Health. 2012;89:915–24.
-
O'Campo P, Dunn JR. Rethinking social epidemiology: towards a science of change. New York: Springer; 2011.
-
Bambra C, Smith KE, Garthwaite K, Joyce KE, Hunter DJ. A labour of Sisyphus? Public policy and health inequalities enquiry from the Blackness and Acheson reports to the Marmot review. J Epidemiol Customs Health. 2011;65(v):399–406.
-
Popay J, Whitehead M, Hunter DJ. Injustice is killing people on a large scale—but what is to be done about it? J Public Health. 2010;32(2):148–ix.
-
Whitehead Thousand, Popay J. Swimming upstream? Taking activeness on the social determinants of health inequalities. Soc Sci Med. 1982;71(7):1234 -1236-1258.
-
Mackenbach JP, Kulhánová I, Menvielle G, Bopp Chiliad, Borrell C, Costa G, et al. Trends in inequalities in premature mortality: a study of 3.two meg deaths in xiii European countries. J Epidemiol Community Wellness. 2015;69(3):207–17.
-
Bor J, Cohen GH, Galea South. Population health in an era of ascent income inequality: USA, 1980-2015. Lancet. 2017;389:1475–90.
-
Nelson Chiliad. Social assistance and EU poverty thresholds 1990-2008. Are European welfare systems providing just and fair protection against low income? Eur Soc Rev. 2013;29(2):386–401.
-
Schrecker T, Bambra C. How politics makes us sick: neoliberal epidemics. London: Palgrave Macmillan; 2015.
-
Stuckler D, Basu S. The body economic: why austerity kills. New York: Basic Books; 2013.
Acknowledgements
Non applicable.
Funding
Equally is supported past the Canada Research Chairs Program. The report was partially funded by the Ontario Ministry building of Customs and Social Services. These funding bodies had no role in the study pattern, data collection, data analysis, data interpretation, or writing of the manuscript.
Availability of data and materials
All information generated or analysed during this study are included in this published commodity (and its additional files).
Writer information
Affiliations
Contributions
Conceptualization: FVS, CR, OSE, As; Search Strategy: FVS, CR; Identification and Pick of the Literature: FVS, CR; Data Extraction and Quality Assessment: FVS, CR; Narrative Synthesis: FVS, CR, OSE, VH, OSE; Drafting of the Manuscript: FVS, CR, OSE, VH, OSE; Study Supervision: AS. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicative. Only published reviews were included in this study.
Consent for publication
Non applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Modified Quality Cess Tool for Quantitative Studies. This file provides a detailed clarification of the tool used to assess the methodological quality of studies included in the systematic review. (DOCX 75 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Eatables Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(due south) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Artistic Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/naught/1.0/) applies to the information made bachelor in this commodity, unless otherwise stated.
Reprints and Permissions
Near this commodity
Cite this commodity
Shahidi, F.V., Ramraj, C., Sod-Erdene, O. et al. The impact of social help programs on population wellness: a systematic review of research in loftier-income countries. BMC Public Wellness 19, 2 (2019). https://doi.org/10.1186/s12889-018-6337-1
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s12889-018-6337-ane
Keywords
- Social assist
- Wellness
- Health inequalities
- Income
- Poverty
- Social policy
- Social welfare
- Socioeconomic status
caballerocound1940.blogspot.com
Source: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-6337-1
0 Response to "Discuss Public Assistance Offered to Low Income Individuals and Families in Your Country"
إرسال تعليق